Who needs extra vitamins? Maybe you. The RDAs are designed to protect healthy people from deficiencies, but sometimes the circumstances of your life (or your lifestyle) mean that you need something extra. Are you taking medication? Do you smoke? Are you on a restricted diet? Are you pregnant? Are you a nursing mother? Are you approaching menopause? Answer “yes” to any of these questions, and you may be a person who needs larger amounts of vitamins than the RDAs provide.
I’m taking medicationMany valuable medicines interact with vitamins. Some drugs increase or decrease the effectiveness of vitamins; some vitamins increase or decrease the effectiveness of drugs. For example, a woman who’s using birth control pills may absorb less than the customary amount of the B vitamins. For more about vitamin and drug interactions.
I’m a smokerIt’s a fact — you probably have abnormally low blood levels of vitamin C. More trouble: Chemicals from tobacco smoke create more free radicals in your body. Even the National Research Council, which is tough on vitamin overdosing, says that regular smokers need to take about 66 percent more vitamin C — up to 100 mg a day — than nonsmokers.
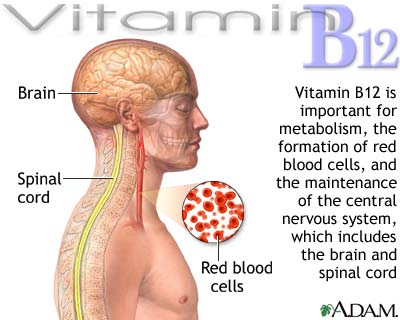
I never eat animalsOn the other hand, if you’re nuts for veggies but follow a vegan diet — one that shuns all foods from animals (including milk, cheese, eggs, and fish oils) — you simply cannot get enough vitamin D without taking supplements. Vegans also benefit from extra vitamin C because it increases their ability to absorb iron from plant food. And vitamin B12–enriched grains or supplements are a must to supply the nutrient found only in fish, poultry, milk, cheese, and eggs.
I’m a couch potato who plans to start working outWhen you do head for the gym, take it slow, and take an extra dose of vitamin E. A study at the USDA Center for Human Nutrition at Tufts University (Boston) suggests that an 800 milligram vitamin E supplement every day for the first month after you begin exercising minimizes muscle damage by preventing reactions with free radicals (parts of molecules) that cause inflammation. After that, you’re on your own: The vitamin doesn’t help conditioned athletes whose muscles have adapted to workout stress.
I’m breast-feedingYou need extra vitamin A, vitamin E, thiamin, riboflavin, and folate to produce sufficient quantities of nutritious breast milk, about 750 milliters (3⁄4 liter) each day. You need extra vitamin D, vitamin C, and niacin as insurance to replace the vitamins you lose — that is, the ones you transfer to your child in your milk.
I’m approaching menopauseInformation about the specific vitamin requirements of older women is as hard to find as, well, information about the specific vitamin requirements about older men. It’s enough to make you wonder what’s going on with the people who set the RDAs. Don’t they know that everyone gets older? Right now, just about all anybody can say for sure about the nutritional needs of older women is that they require extra calcium to stem the natural loss of bone that occurs when women reach menopause and their production of the female hormone estrogen declines. They may also need extra vitamin D to enable their bodies to absorb and use the calcium. Gender Bias Alert! No similar studies are available for older men. But adding vitamin D supplements to calcium supplements increases bone density in older people. The current RDA for vitamin D is set at 5 micrograms/200 IU for all adults, but the new AI (Adequate Intake) for vitamin D is 10 micrograms/400 IU for people ages 51 to 70 and 15 micrograms/600 IU or more for people 71 and older. Some researchers suggest that even these amounts may be too low to guarantee maximum calcium absorption.
Check with your doctor before adding vitamin D supplements. In very large amounts, this vitamin can be toxic.
I have very light skin or very dark skinSunlight — yes, plain old sunlight — transforms fats just under the surface of your skin to vitamin D. So getting what you need should be a cinch, right? Not necessarily. Getting enough vitamin D from sunlight is hard to do when you have very light skin and avoid the sun for fear of skin cancer. Even more difficult is getting enough vitamin D when you have very dark skin, which acts as a kind of natural sunblock. When Centers for Disease Control and Prevention researchers surveyed the vitamin D status of more than 2,000 African American and Caucasian women ages 15 to 49, they found low body levels of vitamin D in 42 percent of the African American women and 4.2 percent of the Caucasian women. Based on these numbers, Boston University researchers suggest that the Recommended Dietary Amount for adults who don’t get enough sunlight may be as much as four times the current recommended amount. Check this out with your doctor; it’s very important news for women who are or hope to be pregnant and need extra vitamin D (check back a few paragraphs for this information).
 Keep in mind that “eating for two” means that you’re the sole source of nutrients for the growing fetus, not that you need to double the amount of food you eat. If you don’t get the vitamins you need, neither will your baby. The RDAs for many nutrients are the same as those for women who aren’t pregnant. But when you’re pregnant, you need extra
Keep in mind that “eating for two” means that you’re the sole source of nutrients for the growing fetus, not that you need to double the amount of food you eat. If you don’t get the vitamins you need, neither will your baby. The RDAs for many nutrients are the same as those for women who aren’t pregnant. But when you’re pregnant, you need extra




 The good news is that vitamin deficiencies are rare among people who have access to a wide variety of foods and know how to put together a balanced diet. For example, the only people likely to experience a vitamin E deficiency are premature and/or low–birth weight infants and people with a metabolic disorder that keeps them from absorbing fat. A healthy adult may go as long as 10 years on a vitamin E–deficient diet without developing any signs of a problem. Aha, you say, but what’s this subclinical deficiency I hear so much about? Nutritionists use the term subclinical deficiency to describe a nutritional deficit not yet far enough advanced to produce obvious symptoms. In lay terms, however, the phrase has become a handy explanation for common but hard-to-pin-down symptoms such as fatigue, irritability, nervousness, emotional depression, allergies, and insomnia. And it’s a dandy way to increase the sale of nutritional supplements.
The good news is that vitamin deficiencies are rare among people who have access to a wide variety of foods and know how to put together a balanced diet. For example, the only people likely to experience a vitamin E deficiency are premature and/or low–birth weight infants and people with a metabolic disorder that keeps them from absorbing fat. A healthy adult may go as long as 10 years on a vitamin E–deficient diet without developing any signs of a problem. Aha, you say, but what’s this subclinical deficiency I hear so much about? Nutritionists use the term subclinical deficiency to describe a nutritional deficit not yet far enough advanced to produce obvious symptoms. In lay terms, however, the phrase has become a handy explanation for common but hard-to-pin-down symptoms such as fatigue, irritability, nervousness, emotional depression, allergies, and insomnia. And it’s a dandy way to increase the sale of nutritional supplements.
 Pantothenic acid, another B-vitamin, is vital to enzyme reactions that enable you to use carbohydrates and create steroid biochemicals such as hormones. Pantothenic acid also helps stabilize blood sugar levels, defends against infection, and protects hemoglobin (the protein in red blood cells that carries oxygen through the body), as well as nerve, brain, and muscle tissue. You get pantothenic acid from meat, fish and poultry, beans, whole grain cereals, and fortified grain products. As with biotin, the Food and Nutrition Board has established an Adequate Intake (AI) for pantothenic acid.
Pantothenic acid, another B-vitamin, is vital to enzyme reactions that enable you to use carbohydrates and create steroid biochemicals such as hormones. Pantothenic acid also helps stabilize blood sugar levels, defends against infection, and protects hemoglobin (the protein in red blood cells that carries oxygen through the body), as well as nerve, brain, and muscle tissue. You get pantothenic acid from meat, fish and poultry, beans, whole grain cereals, and fortified grain products. As with biotin, the Food and Nutrition Board has established an Adequate Intake (AI) for pantothenic acid.